The Dole Institute for Research and Education (IDOR), in collaboration with the Oswaldo Cruz Foundation (Fiocruz) and the Respiratory Research Institute of the Federal University of Rio de Janeiro (UFRJ), has launched the first clinical trial in the country to evaluate the efficacy of extracellular vesicles in the treatment of acute respiratory distress syndrome (ARDS). Extracellular vesicles are microscopic structures that function as part of sophisticated cellular communication systems. This condition is one of the leading causes of intensive care unit admission and death in respiratory infections.
- Movies with dogs: Why do they move us so easily?
- nap: How many hours should it last and who should avoid it? Experts will answer
Researchers say the new study puts the country at the forefront of a new generation of cell therapies, pioneering an approach that could revolutionize the treatment of serious lung diseases and other inflammatory and degenerative diseases.
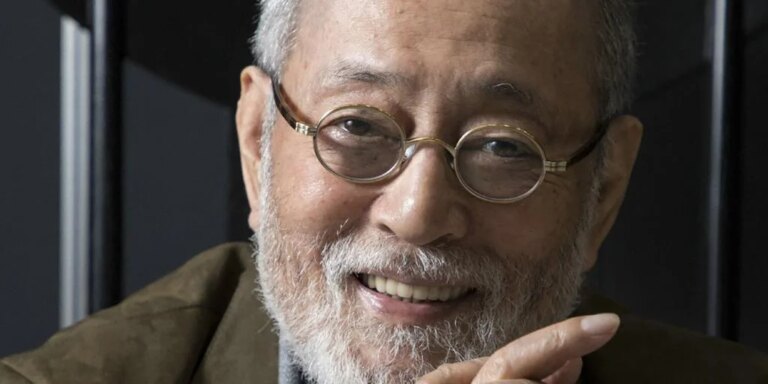
Bruno Solano, researcher, physician and project coordinator at the IDOR Institute for Research and Education (IDOR), said in a statement: “We are living in a historic moment for Brazilian science with the advancement of safe and accessible biotechnological therapies. This therapy was developed in Brazil with excellent technology and has great potential for the treatment of severe lung inflammation.”
This study evaluates the effectiveness of using mesenchymal stem cell-derived extracellular vesicles in treating the condition.
Transports proteins, lipids, and RNA fragments (including microRNAs). MicroRNAs are molecules with the ability to modulate gene activity, which is essential for controlling inflammation and stimulating tissue repair. Based on this knowledge, Brazilian scientists sought safe, scalable, and technologically advanced ways to convert these natural signals into biological medicines.
The vesicles used are derived from human umbilical cord mesenchymal stem cells, which are grown under highly controlled conditions at the IDOR Biotechnology and Cell Therapy Center at San Rafael Hospital in Salvador (BA). The Phase I/II study will involve 15 patients diagnosed with ARDS and admitted to the intensive care unit.
ARDS is a serious and potentially fatal lung disease in which diffuse damage to the alveoli causes respiratory failure and fluid accumulation. It is often caused by conditions such as sepsis, pneumonia, severe COVID-19 infection, or trauma, and requires intensive ICU care. Treatment focuses on treating the underlying cause and supporting respiratory function with mechanical ventilation.
The main objective of the study is to evaluate the safety, tolerability, and possible therapeutic efficacy of intravenous infusion of extracellular vesicles. By acting systemically, the vesicles are expected to control lung inflammation, reduce tissue damage, and promote recovery.
Unlike stem cell therapy, which uses living cells, extracellular vesicle therapy is acellular, or “cell-free,” and is an important innovation in the field of regenerative medicine. Its main benefits include increased product stability and standardization. This not only allows for more controlled production with less batch-to-batch variation, but also significantly reduces the risk of immune rejection.
Furthermore, the high stability of the vesicles greatly facilitates storage and transport, facilitating scalability and use in various clinical situations.
The project, which was conceived as an emergency response to the COVID-19 pandemic, remains extremely important as ARDS can be caused by a variety of conditions, including severe infections and trauma, and could be a critical resource in the event of a new pandemic. The results of this study are expected to pave the way for expanded research, including more institutions and patients participating in Phase 3 of clinical trials.